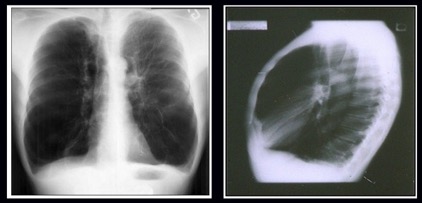
Given these changes from the original case, what is your diagnosis?
What is your diagnostic explanation?
As compared to the long case, this patient is a 62-year-old man who presents to clinic (at the urging of his wife) with exertional dyspnea. He becomes winded after climbing a single flight of stairs. He also reports a nonproductive cough, which he notices primarily at night. His wife states that he awakens from sleep significantly short of breath. He states that his cough and nocturnal dyspnea are much improved when elevating his head with 3-4 pillows. His wife states that his ankles appear swollen. No chest pain. No fever/chills. PMH is significant for hypertension; he admits to frequently forgetting to fill his medications. He is a current smoker with a 40-year pack history. He used to enjoy evening walks with his wife, but no longer exercises due to progressively worsening dyspnea. On exam the patient appears obese, calm, alert, oriented, and in no obvious distress. Temperature is 37C, HR 96, BP 142/92, RR 20. Cardiac auscultation reveals a third heart sound, best appreciated with a bell over the apex. No murmurs or friction rubs. No JVD. Breath sounds are distant on auscultation. Crackles are present over bilateral bases, over which the chest wall is dull to percussion. He has moderate pitting edema up to his ankles bilaterally.