Given these changes from the original case, what is your diagnosis?
What is your diagnostic explanation?
As compared to the long case, this patient is a previously healthy 36-year-old female who presents to a family physician for the first time due to decreased exercise tolerance and exertional dyspnea. She reports: “I really get out of breath when I run, which is not like me.”
HPI: Patient began running for the first time in her life about 6 months ago. She states for the past 2 months she hasn’t been able to run her usual amount of 2 miles at a time. She gets fatigued easily and excessively short of breath after .5 miles which is not her normal. On one occasion when she tried to continue running, she became dizzy and had to stop because she thought she might pass out. She previously attributed this to poor hydration and heat, but now thinks there may be something wrong with her. She does not report any other episodes of presyncope or syncope. She does not report chest pain, palpitations, orthopnea, PND, edema, diaphoresis, nausea, cough, or fever. Prior to these last few months, she does not report any episodes of presyncope, exertional dyspnea, or low exercise tolerance; however, she never participated in sports or exercise until recently.
PMH: No known medical conditions. This is the first time she has seen a physician since she was an adolescent.
SH: Single, without children, works as a dental hygienist. No tobacco or illicit drugs. Drinks socially with her friends on weekends. Eats a well- balanced diet.
FMH: Family is healthy with no medical problems.
Physical Examination:
VS- BP 120/80 mmHg, P 68, RR 12, BMI 24 kg/m2
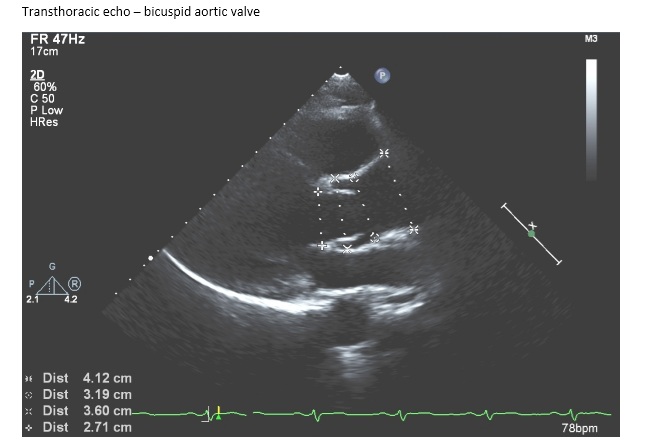
CV- RRR, S1 normal intensity, S2 soft and singular with inspiration, Grade II/VI systolic ejection murmur heard best at right second intercostal space and transmitted to carotid arteries.
No clubbing, cyanosis, or edema. No bruits.
Resp- Clear to auscultation bilaterally, no wheezing, rales, or rhonchi. No dullness to percussion.
Rest of exam is WNL