Given these changes from the original case, what is your diagnosis?
What is your diagnostic explanation?
As compared to the long case, this patient is a 49-year-old female who presents to her PCP with a 3 month history of increasing exertional dyspnea. She reports: “I get really out of breath whenever I try to do anything these days.”
HPI: Onset was gradual and not associated with a specific event, but is more noticeable with activities like yard work, climbing stairs, and grocery shopping. It is associated with fatigue and weakness that has caused her to want to avoid precipitating activities. Dyspnea is relieved with 5-10 minutes of rest and is not associated with chest pain, palpitations, lightheadedness, diaphoresis, nausea, syncope, cough, or fever. Patient does not report orthopnea (sleeps on one pillow), paroxysmal nocturnal dyspnea, or LE edema.
PMH:
Conditions- Hypertension, hypercholesterolemia, obesity, type II DM
Medications- Metformin, HCTZ, Atorvastatin, Levonorgestrel IUD
Surgeries- None
SH: Patient is a 45 pack year smoker, is a social drinker, and has never used illicit drugs. Patient does a lot of cooking for her family consisting of meat, potatoes, cheese, casseroles, vegetables, etc. Patient does not exercise.
FMH: Family history of hypertension, hypercholesterolemia, obesity, and type II DM in both her maternal and paternal families. Father died at age 55 from MI. Paternal grandfather had a stroke at age 65 and died from MI at age 67. Children are 21 and 27 and healthy.
ROS: No significant findings
Physical Examination:
VS- BP 145/95 mmHg, P 72, RR 16, BMI 38 kg/m2
CV- RRR, S1, S2, no S3/S4, no murmurs, no bruits, no JVD, no cyanosis, no clubbing, no peripheral edema
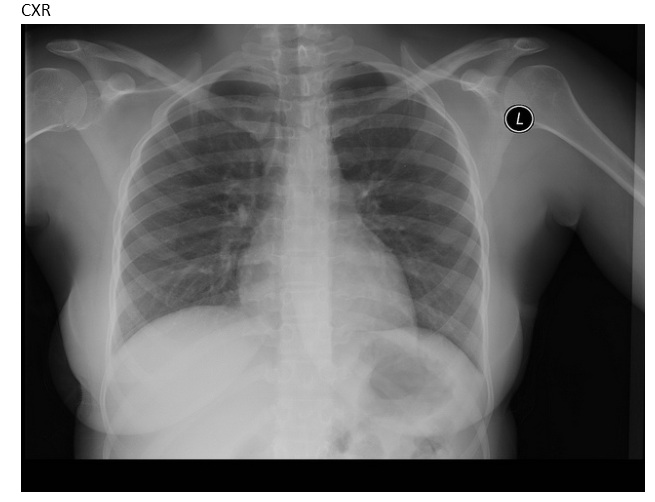
Resp- Lungs clear to auscultation bilaterally, no wheezing, rhonchi, or rales. No dullness to percussion.
Rest of exam is normal