Given these changes from the original case, what is your diagnosis?
What is your diagnostic explanation?
As compared to the long case, this patient is a 22 year old, previously healthy female presenting to the Emergency Department with acute onset sharp, pleuritic, substernal pain that radiates to her left shoulder (trapezius ridge).
HPI: The patient reports that the pain began while she was lying in her bed reading 3 hours ago. Pain intensity increases when supine and decreases with sitting forward. Patient reports no prior occurrences. Pain is not associated with palpitations, nausea, diaphoresis, meals, cough, fever, or anxiety. Patient has no history of DVTS or coagulopathy, recent travel, surgeries, or leg swelling/pain/erythema. No history of malignancy, autoimmune disorder, myocardial infarction, or cardiac surgery reported.
ROS: Weight loss of 8 pounds in 6 months without trying associated with decreased appetite. Myalgias present off and on for past 6 months. 1/10 joint pain in MCP and IP joints of both hands. Face rash with sun exposure that was always thought to be a sunburn.
PMH: Raynaud phenomenon
FMH: Father has rheumatoid arthritis
PE:
VS- BP 118/62 mmHg, P 110, RR 14, T 98.6 F, BMI 21 kg/m2
HEENT- Erythema in a malar distribution over the cheeks and bridge of the nose
CV- RRR, S1 and S2 normal intensity, no S3/S4/murmur. Pericardial friction rub present (superficial scratchy sound best heard with the diaphragm over the left sternal border). No JVD or distant heart sounds. Pain is not reproduced with palpation of chest
Resp- Clear to auscultation bilaterally
Abdomen- Bowel sounds present, soft, non-tender, non-distended
MS- No joint erythema or swelling, 5/5 muscle strength throughout, muscles non-tender to palpation, full range of motion throughout.
Tests:
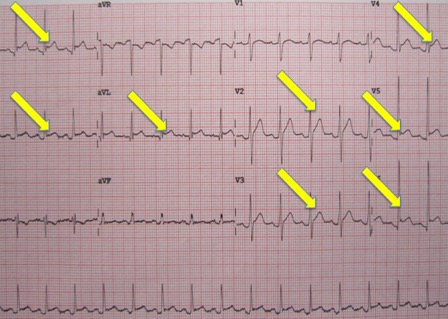
ECG- See below
CXR- See below
Echo- See below